Supercharge your data platform
Automated workload management is here
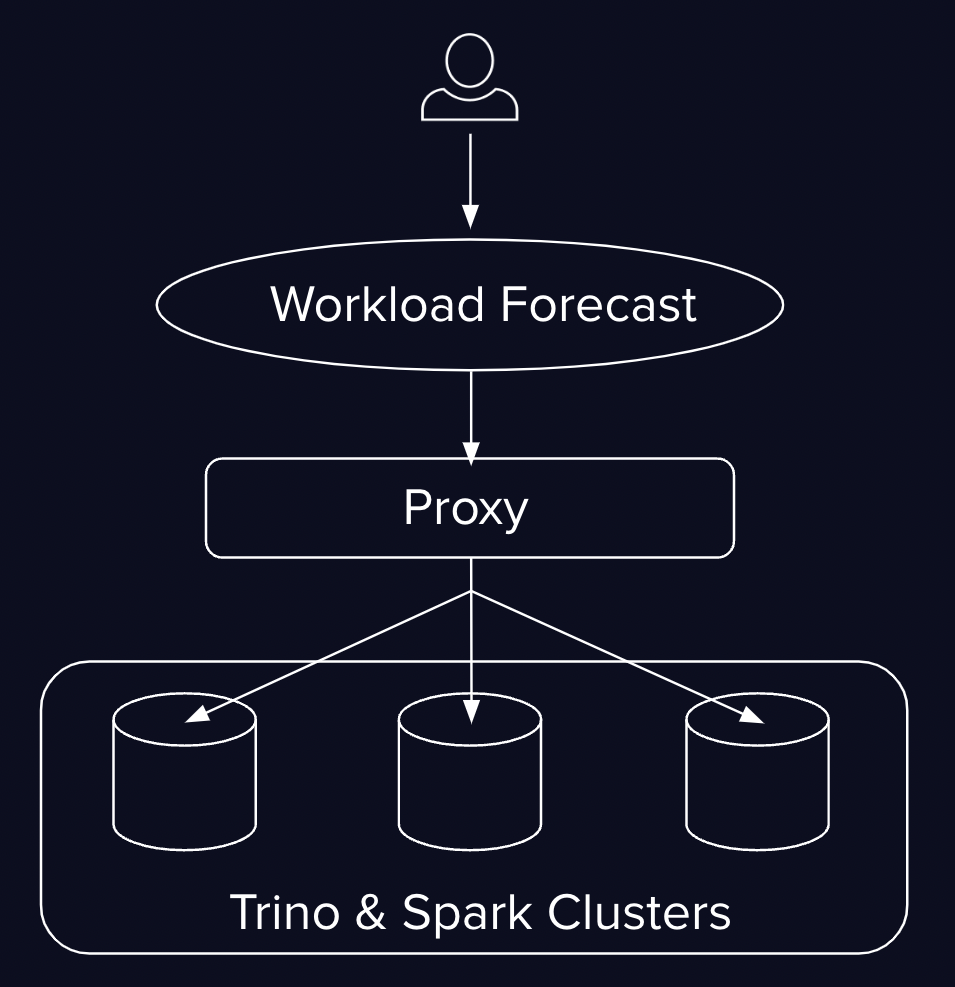
InQuery is a smart reverse proxy that routes queries across your Trino and Spark clusters.

Optimizing your data platform is hard
Enterprise lakehouse deployments suffer from...
High
Server costs
Query latency
Management overhead
Query failure rates
Operational overhead
Low
Resource efficiency
System visibility
Analyst productivity
Query Workload Estimation
InQuery uses AI to predict CPU and Memory needs for incoming queries based on historical traffic patterns.
Resource-aware query routing
InQuery dynamically directs queries to the best-suited engine and cluster based on real-time resource availability.
Proactive Execution Limits
InQuery leverages query resource predictions to preemptively reject queries that exceed specified execution limits.
Workload Translation
InQuery translates workloads across SQL dialects so that your users can have an engine-agnostic querying experience.
Data Platform Performance Improvements Upwards of
40%
Cluster CPU Utilization
25%
Query Engine Compute Costs
40%
Query Latency Improvement
Book a Demo
Book a demo with InQuery to see how we can help you provide a better data platform experience to your users.






